Bariatric Center Adds Duodenal Switch Surgery
 Patients with a BMI ≥50 are good candidates for duodenal switch surgery.
Patients with a BMI ≥50 are good candidates for duodenal switch surgery.
It is well documented that patients who have a BMI ≥30 are at risk of premature death due to significant obesity-related comorbid conditions, including cardiovascular disease, degenerative joint disease, hypertension, sleep apnea, stroke and Type 2 diabetes.
“Equally, a growing body of research suggests lifestyle and behavior changes do not result in sustained, significant weight loss for these patients,” said Keenan R. Berghoff, MD, FACS, medical director of Bariatric Surgery at North Kansas City Hospital and a general surgeon with Meritas Health Comprehensive Surgery.
Physicians can refer these patients to NKCH’s Bariatric Center for proven surgical weight loss options, including the hospital’s newest option, the laparoscopic modified duodenal switch surgery.
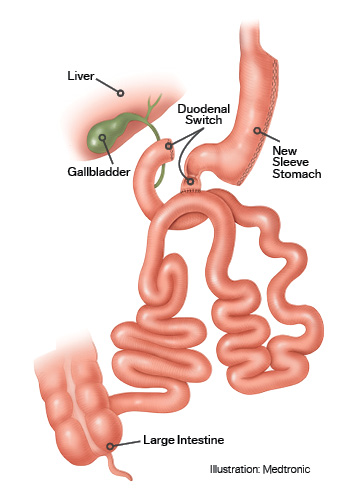
Laparoscopic Modified Duodenal Switch
Dr. Berghoff performs the laparoscopic surgery, which combines both restrictive and malabsorptive methods in patients with Class III obesity (BMI ≥50). Dr. Berghoff has specialized training in advanced laparoscopic surgery and bariatric procedures.
“The duodenal switch procedure reduces the stomach size and manipulates the way food travels through the GI tract,” Dr. Berghoff said. “This leads to less caloric absorption and sustained weight loss. Stomach capacity is reduced to about 4-6 ounces, and patients lose about 20% more weight than they would with gastric bypass surgery.”
The 90-minute surgery combines components of both the gastric sleeve and gastric bypass procedures in three ways:
- About 75%-80% of the stomach is removed, which creates a tube-shaped stomach much like the gastric sleeve procedure, and the pylorus remains attached to the duodenum
- The duodenum is then divided into two sections, leaving the first portion connected to the outlet of the newly created stomach
- The remaining small intestine is reconnected to the duodenum so bile and digestive enzymes mix back into the food stream
“Although not a new procedure, the modified duodenal switch technique has improved greatly,” Dr. Berghoff said. “Patients previously were left with malabsorptive issues such as diarrhea, but those have been eliminated. The risks now associated with bariatric surgery are on the order of those for an appendectomy, hernia repair or a hysterectomy. Given the comorbid conditions associated with obesity, the risk of not doing surgery is 10 times higher than doing surgery.”
Bariatric Surgery Candidates
To be considered for bariatric surgery at NKCH, patients are required to meet a number of criteria. In most cases, they should:
- Have a BMI ≥35; they may qualify with a lesser weight if there are serious medical problems that could be corrected or greatly improved with significant weight loss
- Have the intellectual capacity to understand and comply with the recommended postoperative program
- Have a history of failing to lose weight or maintain weight loss on other diet programs
- Not have any medical conditions that would make the surgical risks prohibitive or inappropriate
- Demonstrate a willingness to engage in lifestyle and nutritional habits known to support weight loss
Comorbidity Changes
According to the National Institute of Diabetes and Digestive Kidney Diseases, bariatric surgery offers long-lasting, effective weight loss and improved control of blood glucose levels. Dr. Berghoff noted patients who undergo the modified duodenal switch often see a reversal in their diabetes, and those who have sleeve or bypass surgery can expect resolution of their diabetes more than 60% of the time.
“We’re changing the metabolism of these patients and thus the pathophysiology of their diabetes,” Dr. Berghoff added. “Surgery is the best choice obese patients have for diabetes resolution.”
He pointed to the American Diabetes Association’s Standards of Medical Care in Diabetes — 2018 recommendation that metabolic surgery be an option:
- To treat Type 2 diabetes in appropriate surgical candidates with a BMI ≥40 regardless of the level of glycemic control or complexity of glucose-lowering regimens and in adults with a BMI 35.0-39.9 when hyperglycemia is inadequately controlled despite lifestyle changes and optimal medical therapy
- For adults with Type 2 diabetes and a BMI 30.0-34.9 if hyperglycemia is inadequately controlled despite optimal medical control by either oral or injectable medications (including insulin)
Bariatric surgery and the resulting weight loss help people increase their activity and quality of life, but it also can result in a number of significant health benefits:
- 89% reduction in five-year mortality rate
- 80% of diabetes resolved
- 75% of hypertension resolved
- 70% of elevated cholesterol levels normalized
- 90% of weight loss maintained beyond 10 years
Nutrition
Patients follow a five-day high-protein, liquid diet prior to surgery, which reduces the size of the liver and allows for a more successful operation. After surgery, they stay on liquids for seven days and then add foods over seven weeks:
- Week 1: Soft foods (e.g., Greek or light yogurt, low-fat cottage cheese, sugar-free pudding, pureed soups)
- Week 2: Soft solid foods (e.g., avocado, eggs, reduced-fat cheese, tofu)
- Week 3: Beans, deli-shaved meats, fish, lentils, shellfish, soft cooked vegetables, soft fresh fruit, soup
- Week 4: Cooked vegetables with skin, ham, lean ground beef and poultry, raw salad greens, soft fruits with skin
- Week 5: Corn, oatmeal, poultry, potatoes, raw fruits and vegetables, whole grains
- Week 6: Dried fruit, nuts, peanut butter
- Week 7: Citrus fruits, beef, pickled foods, pork, protein bars, vegetable juices, seeds, wild game
Hydration is vital for all bariatric surgery patients, and patients are asked to drink a minimum of 64 ounces of fluids daily.
Because manipulation of the gut alters the natural absorption of nutrients, patients take over-the-counter bariatric multivitamins and calcium supplements. Patients who have the switch surgery also take vitamin K.
Support
People interested in bariatric surgery must attend a free informational seminar held regularly at NKCH prior to surgery. Dr. Berghoff leads the seminar and answers questions to help prospective patients determine if bariatric surgery is right for them.
Patients consult with Dr. Berghoff and the bariatric team for approximately three visits prior to surgery, but some insurance companies require more frequent visits.
In addition to having support from Dr. Berghoff, nurses, a nurse practitioner and dietitians, patients also meet with a psychiatrist
Other Bariatric Surgeries
In addition to the duodenal switch surgery, Dr. Berghoff performs two other minimally invasive bariatric procedures: gastric bypass and gastric sleeve.
With gastric bypass, he bypasses part of the digestive system and reroutes part of the small intestine to connect to a new, smaller stomach pouch.
With gastric sleeve, he removes a large portion of the stomach, which results in a smaller “sleeve”-shaped stomach that restricts the amount of food the stomach can hold.
With all three procedures, patients return home the next day.
Keenan R. Berghoff, MD, FACS
Dr. Berghoff earned his medical degree from Indiana University. He completed his general surgery residency at the University of Missouri and a fellowship in advanced laparoscopy at the Texas Endosurgery Institute.